When it comes to anxiety, it seems like there’s no limit to the symptoms it can cause. So if it seems like you’re running to the bathroom every time you’re extra stressed or anxious, it’s definitely not a coincidence. An anxious stomach can trigger all kinds of uncomfortable digestive symptoms. The stress hormones that your body produces when you’re feeling anxious are known to have a direct effect on the gut, causing symptoms like nausea, abdominal pain, diarrhea, and indigestion. Over time, stress can lead to an imbalance in certain areas of the digestive system making it more likely you’ll develop more serious digestive problems, like IBS or colitis.
Fortunately, there are ways to manage symptoms of an anxious stomach. In this blog post, we will explore the connection between anxiety and IBS, and discuss some holistic ways to improve both conditions!
How stress affects your gut
When we are stressed, the body releases hormones such as cortisol and adrenaline that activate the fight or flight response. This results in increased heart rate, blood pressure, and tightness of the stomach muscles. These physical changes can trigger stomach pain and stress related diarrhea (sometimes called nervous poops).
In addition to the physical effects of stress on the digestive system, our mental health can have a profound effect on the gut as well. Stress and anxiety affects our ability to produce stomach acid and digestive enzymes, which are necessary for breaking down food and absorbing nutrients (1).
If stress and anxiety are affecting your gut, you might feel:
- Abdominal pain or cramping
- Bloating
- Diarrhea or constipation
- Gas
- Indigestion
Chronic stress can also lead to an overgrowth of bad bacteria in the gut, which can further contribute to digestive issues.
Related: Do Probiotics Help with Bloating?
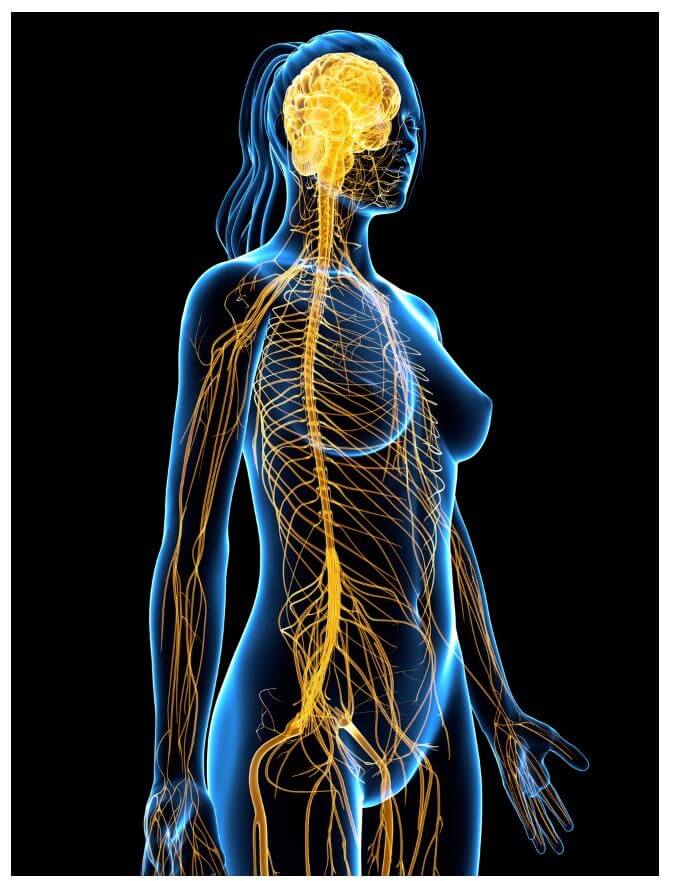
The gut-brain axis
The gut-brain axis (or gut-brain connection) refers to the two-way communication pathway between your brain and your digestive system. Your gut actually has its own nervous system—called the enteric nervous system—that hormones, immune cells, neurons, and gastrointestinal cells use to interact amongst themselves, and the brain.
A poorly functioning gut has been linked to mental health problems, including anxiety and depression. This is because your brain depends on nutrients and neurotransmitters that (in many cases) can only be made in the gut (2).
For example, the vast majority of serotonin—a neurotransmitter responsible for feelings of wellbeing—is made in the gut (3). If there’s not enough serotonin produced in the gut, you may not have enough in the brain to calm anxious thoughts and feelings.
Can stress & anxiety cause more serious gut problems?
The answer is yes! Stress and anxiety can result in more serious digestive diseases, such as ulcerative colitis and irritable bowel syndrome. In fact, there is strong evidence to suggest that stress can trigger flares of these inflammatory bowel conditions. (4)
Chronic psychological stress may lead to an increase in intestinal permeability, or “leaky gut”. Leaky gut occurs when the tight junctions between the cells of our digestive tract become impaired, allowing undigested food particles and other toxins to enter into our bloodstream. This can trigger an inflammatory response in the body and lead to a multitude of systemic symptoms.
Read more: Have A Messed Up Gut? It Could Mean Trouble for Your Mental Health
Anxiety and IBS
Gut disorders, especially IBS, can begin with negative thinking, stress, and anxiety—not just food. Sometimes, a healthy, balanced diet and lifestyle are not enough to prevent or manage symptoms of IBS. In fact, many experts say it’s not possible to effectively treat IBS without addressing anxiety as part of treatment (5).
IBS patients are also more likely to have anxiety or other mental health issues. In one study, 44% of patients with IBS also had anxiety, and 84% had depression. In people without IBS, the prevalence of anxiety and depression was 8% and 6%, respectively (6).
People with IBS may be more sensitive to stress
For some people, environmental, mental, and emotional stress may activate a hypersensitive stress response in the digestive tract that’s difficult to turn off.
Stress & anxiety don’t directly cause a digestive disease, but intense emotions can trigger chemicals in the brain that cause receptors in your gut to be hypersensitive to the body’s stress response.
How can I stop anxiety from causing an upset stomach?
Start by figuring out what causes stress in your life. This will look differently for everyone, and the culprits may be things you don’t suspect.
Then, try keeping a log of symptoms and your emotional state at the time. Make a note if something else occurred that day or the day prior, like a fight with a family member, stress at work, etc.
If you don’t already have steps in place to cope with stress, it’s important to work on a stress management plan asap. Once anxious feelings are under control, your gut will likely begin to calm down as well.
You can also try these to avoid anxiety and keep your gut healthy:
- Add a stress-reducing exercise a few times per week, like yoga, walking, or tai chi. Be mindful of overtraining, and know when to rest.
- Get 7 to 8 hours of sleep per night. Adequate sleep is key to rebalance healthy gut function.
- Talk with your doctor to develop a plan for when you experience a flare-up of gastrointestinal symptoms, especially if they’re severe. Having a plan can decrease the stressfulness of the situation somewhat.
- Avoid coffee. Caffeine and alcohol are gut irritants for many people. Coffee can also worsen diarrhea symptoms, especially if you already have an anxious gut.
- Avoid fried or fatty foods. Very high fat foods can be hard to digest, and put strain on an already stressed out gut.
- Add pre- and probiotics to your diet to fight pro-inflammatory bacteria. You can take a supplement, or include fermented vegetables, kefir, yogurt, or take a high-quality probiotic supplement.
- Know the benefits and risks of different symptom-relieving medications. Your doctor can help you decide when to rely on a little extra support.
Talk with an integrative physician who has experience with stress-related digestive problems
While it’s impossible to pinpoint what causes every flare up of digestive upset, we do know there’s a strong connection between stress, anxiety, and an unhappy gut. If you have a gut that’s sensitive to stress & anxiety, it’s likely you’ll experience symptoms as a result of stressful situations. The best way to deal with these flare ups proactively is to actively manage stress.
If you have a stressed out gut, there are numerous practices that are effective for not only reducing stress but also providing relief from digestive upset too. If you’re still struggling with inflammatory bowel problems, talk with an experienced integrative medicine doctor who can help you find relief from your symptoms.
Resources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC26223/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5641835/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5526216/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6821654/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4202343/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5733421/



