PCOS & Diabetes: The Link Between Hormones and Insulin Resistance
Polycystic ovarian syndrome (PCOS) affects the endocrine system in ways that can cause insulin resistance and blood sugar imbalances. These two things are significant risk factors for developing diabetes, even if you’re at a healthy weight. If you have PCOS, it’s important to be aware of diet and lifestyle factors that affect your blood glucose levels, even if your PCOS symptoms are under control. In a moment, you’ll understand why diabetes occurs more often in PCOS patients, and what you can do to prevent impaired glucose tolerance now, and in the future.
Learn to manage your hormones naturally with diet and lifestyle when you join my community, the Superwoman Circle.
What Is PCOS?
Polycystic ovarian syndrome (PCOS) is a condition that affects hormones, causing irregular periods, fertility problems, and cysts on the ovaries. These symptoms are caused by an imbalance in the hormones estrogen and progesterone, and the excess production of androgens, or male hormones, like testosterone.
High levels of insulin are also a root cause of PCOS, and cause the ovaries to make excess testosterone, which interferes with ovulation and causes some of the symptoms of PCOS like excess hair growth, thinning of hair on the head, and acne.
Excess weight is due in part to aspects of insulin resistance which, although not present in every single case of PCOS, is very common (1). Though weight struggles are common with PCOS, lean women can also experience PCOS.
Read: 9 Unexpected Symptoms of PCOS to Watch
Untreated PCOS increases risk of some health problems
Long term, PCOS left untreated can lead to metabolic syndrome, type 2 diabetes, and cardiovascular disease due to chronic inflammation and impaired glucose tolerance, so there’s much incentive to address the lifestyle, diet, and hormonal factors that play a part in PCOS.
Even if you’re managing PCOS symptoms with something like hormonal birth control pills, this doesn’t address the underlying metabolic issues that place you at higher risk for chronic issues like type 2 diabetes.
Watch: Testing for the PCOS Triangle
Signs & Symptoms of PCOS
Despite its name, you do not have to have cysts on your ovaries to have PCOS. The name itself creates confusion for many women, but cysts aren’t always present.
The primary symptoms of PCOS are:
- Body hair (called hirsutism)
- Weight gain or obesity, despite a healthy and active lifestyle
- Infertility
- Not ovulating
- Acne, especially on the back and chest
- Hair loss, or thinning hair on the head
- Irregular periods or no period (dysmenorrhea, or amenorrhea)
- Ovarian cysts
- Estrogen dominance signs (like worsening PMS, painful periods)
- Anxiety and depression
At your doctor’s office, PCOS is diagnosed by having two of the following: excess androgens (testosterone), polycystic ovaries, and ovulatory dysfunction.
Related: Can PCOS Be Cured? 9 PCOS Myths Debunked
What to know about PCOS and diabetes
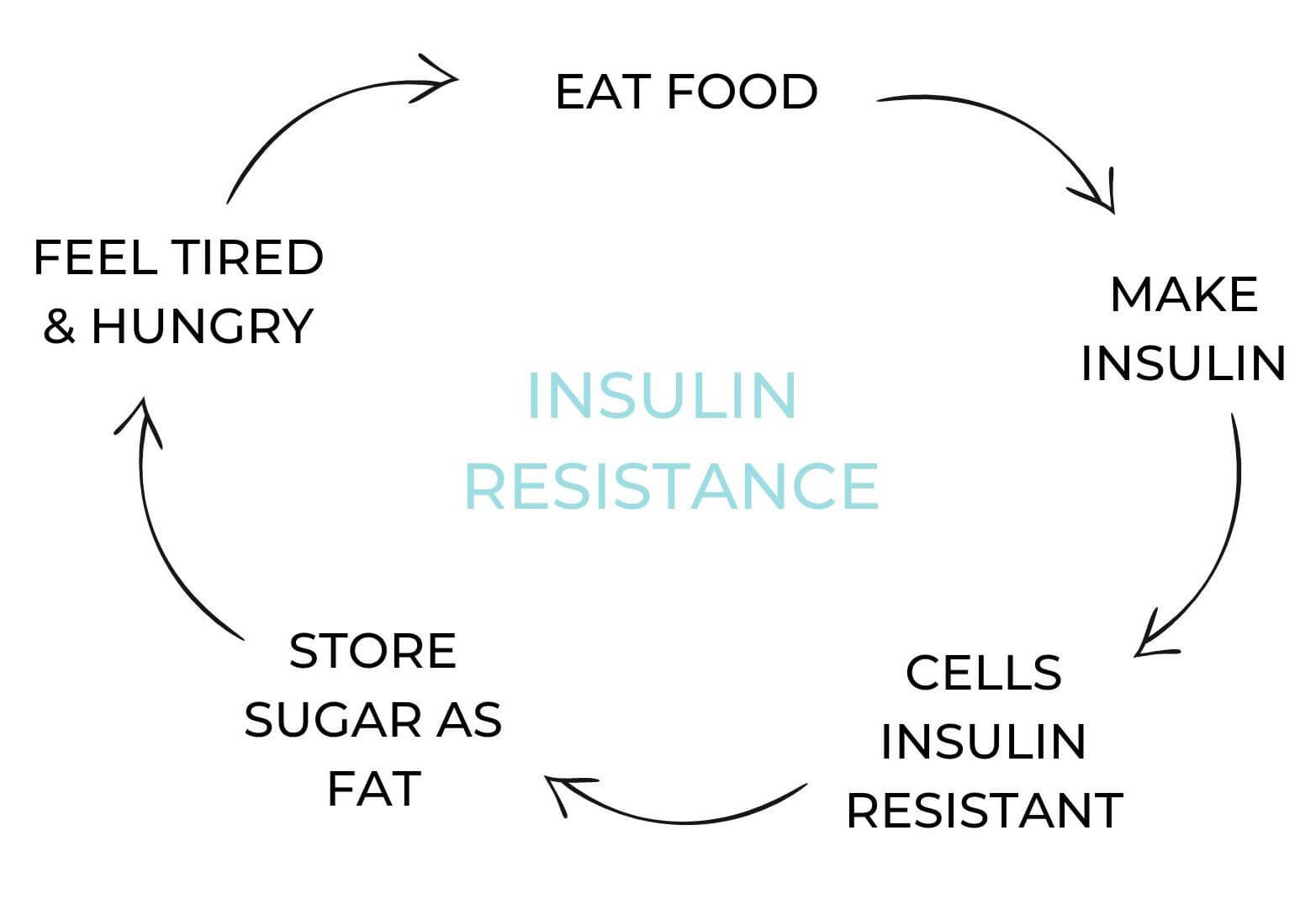
With PCOS, I often see insulin resistance, where insulin levels remain too high for too long, because the cells aren’t responding to their message.
This is a problem for a few reasons:
One, for fertility. High levels of insulin can interfere with ovulation. Too much insulin causes the ovaries to produce more testosterone than normal, which interferes with healthy follicle development (where eggs are made in the ovaries) and prevents ovulation. Without ovulation, pregnancy cannot occur.
Two, for metabolic health. When insulin is constantly high, it becomes pro-inflammatory and can lead to weight gain, type 2 diabetes, and even heart disease.
Three, for energy levels. When blood sugar isn’t balanced and insulin isn’t functioning optimally, you can feel tired, run down, and have low energy levels overall.
How PCOS affects blood glucose
PCOS is linked with blood sugar imbalances, mainly because of a decline in the body’s sensitivity to insulin. To break this down, let’s clarify how insulin affects blood sugar.
Blood sugar is a measurement of glucose in your bloodstream. It rises after you eat, and goes down as your cells use the glucose for energy. But the glucose needs a helper to make it inside the cell, and insulin is like the key that allows glucose to open the door.
Because PCOS can make the body less sensitive to the message insulin sends, this results in blood glucose levels remaining elevated for a longer period of time. Over time, elevated blood sugar increases inflammation and the risk of serious metabolic health issues.
Related: How to Lose Weight with PCOS + 10 Easy Tips to Start
Is inflammation to blame for blood sugar imbalance?
Recent evidence suggests that inflammation may actually cause the insulin resistance that’s common with PCOS, rather than insulin resistance being a result of PCOS itself (2).
We already know that chronic inflammation causes blood sugar imbalance. Everything from an underlying infection to high rates of stress contributes to this kind of inflammation.
Inflammation is a big problem for your blood sugar because it makes it harder for insulin to do its job—which is to allow sugar inside the cell to use as energy.
Read: PCOS and Leaky Gut? The Gut-Hormone Connection
Can untreated PCOS cause diabetes?
More than half of women with PCOS develop type 2 diabetes by age 40. PCOS is one of the main conditions that can lead to insulin resistance and type 2 diabetes (3). This can occur even past a woman’s reproductive years, which is why it’s important to address PCOS symptoms even if you’re not concerned about fertility.
Chronic inflammation from PCOS can cause the body to become less sensitive to insulin over time. When this happens, blood sugar becomes elevated and inflammation increases, setting the stage for type 2 diabetes.
Fortunately, there are things you can do to treat PCOS and improve insulin sensitivity.
Natural ways to improve insulin sensitivity with PCOS
There are many natural ways to improve insulin sensitivity and help reverse PCOS symptoms.
Eat an anti-inflammatory diet
Plenty of nutrient-dense veggies, healthy omega-3 fats, and quality protein will serve your blood sugar and hormone balance best. Try these 6 easy PCOS diet recipes to get started.
Keep blood sugar balanced
Since insulin dysregulation is at the heart of PCOS, get healthy carbohydrates from low starch plant foods (greens, broccoli, berries, etc.), and keep processed grains to an absolute minimum. You’ll want to omit added sugar, alcohol, and maybe even gluten, depending on your tolerance.
Hormone-metabolizing greens
Cruciferous veggies like broccoli, cauliflower, leeks, and kale help the body metabolize excess hormones. Aim for about 8 servings per week for healthy hormones.
Exercise
Daily! Thirty minutes of moderate cardio, strength training, or yoga is worth its weight in gold for decreasing inflammation, improving stress markers, and maintaining a healthy response to insulin. No need to overdo it, though, as overexercising can increase cortisol production in the same way as stress.
Work on gut health
New studies are showing that our microbiome plays a role in hormone balance and PCOS symptoms.
Use the right supplements

- Berberine supports a healthy response to insulin, keeping blood sugar balanced and healthy (4).
- Saw palmetto inhibits the enzyme that converts hormones to testosterone, which can alleviate unwanted body hair, and help with healthy hair growth on your head (5).
- Magnesium helps mediate metabolic syndrome, which is a collection of symptoms involving high blood pressure, blood sugar imbalance, body fat around the waist, and high triglycerides (6).
- Myo-inositol reduces androgens, supports ovarian function, and insulin sensitivity (7,8,9).
- Maca helps to support estrogen production, energy, and vitality
- Omega-3s are powerful for reducing inflammation and promoting healthy cholesterol levels.
Hormone Helper now contains maca, myo-inositol, and saw palmetto to support a balance between estrogen, testosterone, and progesterone.
Learn more about the best supplements for PCOS.
Other ways to reduce insulin resistance with PCOS
Reduce stress. High stress levels ramp up inflammation which makes it harder for insulin to do its job of lowering blood glucose. Having activities that help you relax is incredibly important for your overall health and fertility.
Get enough sleep. Most people need around eight hours per night. Consider going to bed and waking up at the same time each day to help support your circadian rhythm.
Reduce environmental toxins. Toxins like pesticides, herbicides, and BPA can disrupt hormone function and increase inflammation. Choose organic foods when possible, and avoid plastic water bottles.
What to remember
Those with polycystic ovarian syndrome are at increased risk for metabolic issues like type 2 diabetes. If you have PCOS, maintaining healthy blood glucose levels are important to reduce this risk, as well as help you manage the range of PCOS symptoms such as hair loss, high testosterone levels, and weight gain. Because evidence suggests that inflammation may be at the root of PCOS, diet and lifestyle choices to reduce inflammation and keep stress low are the best places to focus your energy.
Resources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5672719/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3309040/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3425413/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2410097/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2840915/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4198467/
- https://www.ncbi.nlm.nih.gov/pubmed/18335328
- https://www.ncbi.nlm.nih.gov/pubmed/17952759
- https://www.ncbi.nlm.nih.gov/pubmed/18854115
